Introduction
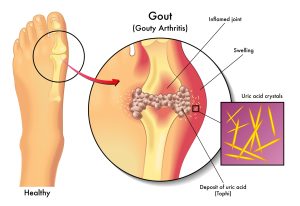
Gout, a form of inflammatory arthritis, presents itself with sharp pain and swelling in the joints, most commonly affecting the big toe. This comprehensive guide aims to simplify the complexities of gout, unraveling its symptoms, causes, diagnosis, and practical management approaches.
Symptoms
Gout manifests through episodes known as flares or attacks. Recognizing these symptoms is crucial for timely intervention:
- Intense Pain: The hallmark of a gout attack is excruciating pain in the affected joint, often striking suddenly and intensifying over a few hours.
- Swelling: The affected joint swells, becoming visibly larger and sometimes accompanied by warmth and redness.
- Discoloration or Redness: Gout can cause the skin over the affected joint to turn red or even purple, indicating inflammation.
- Stiffness: Joints affected by gout may become stiff, limiting their range of motion.
- Tenderness: Even the lightest touch, such as a bedsheet covering the joint, can cause discomfort.
- Warmth or “On Fire” Sensation: The affected joint may feel unusually warm or give off a sensation of being on fire.
These symptoms can persist for a week or two during a gout attack, with intermittent periods of relief between episodes.
Causes
Understanding the causes of gout is pivotal for effective management. Gout occurs due to an accumulation of uric acid in the body, leading to the formation of sharp crystals in the joints. The primary contributors to elevated uric acid levels include:
- Dietary Factors: Foods high in purines, such as organ meats, game meats, certain seafood, and sugary drinks, can contribute to increased uric acid levels.
- Genetics: A family history of gout increases the likelihood of developing the condition.
- Health Conditions: Conditions like obesity, congestive heart failure, diabetes, hypertension, kidney disease, and blood cancer elevate the risk of gout.
- Gender and Age: Men are three times more likely to develop gout, and women typically experience it after menopause.
- Medications: Certain medications, including diuretics and immunosuppressants, can influence uric acid levels.
Diagnosis and Tests
Diagnosing gout involves a combination of clinical assessments and tests. Healthcare providers conduct a physical examination, inquire about symptoms, and may use imaging tests, such as X-rays, ultrasounds, and MRIs, to assess joint conditions. Additionally, blood tests measuring uric acid levels and joint aspiration, involving the extraction of fluid from the joint, contribute to a comprehensive diagnosis.

Management and Treatment
Effectively managing gout requires a multifaceted approach, addressing both symptom relief and long-term prevention. Key components of gout management include:
- Symptomatic Relief: During flares, nonsteroidal anti-inflammatory drugs (NSAIDs), colchicine, and corticosteroids can provide relief from pain and inflammation.
- Medications to Lower Uric Acid Levels: Drugs such as allopurinol, febuxostat, pegloticase, and probenecid are commonly prescribed to lower uric acid levels and reduce the frequency of gout attacks.
- Low-Purine Diet: A dietary shift involving reduced consumption of high-purine foods helps in managing uric acid levels. (want to explore more treatments for different health problems)
Prevention
Taking proactive steps to prevent gout attacks is crucial for individuals with the condition. Strategies include:
- Dietary Modifications: Limiting intake of high-purine foods like organ meats, seafood, and sugary drinks.
- Hydration: Adequate water intake supports kidney function, aiding in the elimination of uric acid.
- Regular Exercise: Engaging in regular physical activity reduces stress on joints and lowers the risk of obesity, a contributing factor to gout.
Outlook / Prognosis:
Understanding the outlook for individuals with gout provides insights into what to expect:
- Recurrent Flares: Gout typically involves recurrent flares, but effective management strategies can significantly reduce their frequency.
- Complications: Untreated gout may lead to permanent joint damage, tophus formation (buildup of uric acid in joints and soft tissue), kidney stones, and heart disease.
- Treatment Effectiveness: Gout is treatable. Individuals maintaining blood uric acid levels below 6 mg/dL are less likely to experience severe attacks.
Living With Gout
Living with gout involves adopting practical strategies to manage attacks and enhance overall well-being:
- During Gout Attacks: Avoiding alcohol and sugary drinks, staying hydrated, elevating affected joints, and applying ice packs can alleviate symptoms.
- Seeking Healthcare: Consult a healthcare provider promptly if experiencing intense joint pain, swelling, or changes in symptoms.
Conclusion
In conclusion, demystifying gout empowers individuals to navigate this challenging condition effectively. By understanding symptoms, causes, and adopting proactive management strategies, those with gout can enhance their quality of life and minimize the impact of recurrent flares.