Autoimmune diseases represent a diverse group of disorders characterized by the immune system erroneously attacking the body’s own tissues. This aberrant immune response can lead to chronic inflammation, tissue damage, and a variety of clinical manifestations depending on the specific disease. Over the past few decades, significant advances have been made in understanding the pathophysiology of autoimmune diseases, leading to the development of novel therapeutic strategies. This article delves into the recent advances in treating autoimmune diseases, with a focus on targeted therapies, biologics, and personalized medicine.
Understanding Autoimmune Diseases
Autoimmune diseases affect millions of people worldwide, with conditions such as rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), multiple sclerosis (MS), and type 1 diabetes mellitus (T1DM) being among the most prevalent. The pathogenesis of these diseases involves a complex interplay between genetic predisposition, environmental triggers, and immune system dysregulation. Traditional treatment options have primarily focused on broad immunosuppression to mitigate the immune response. However, these approaches often come with significant side effects and do not address the underlying cause of the disease.
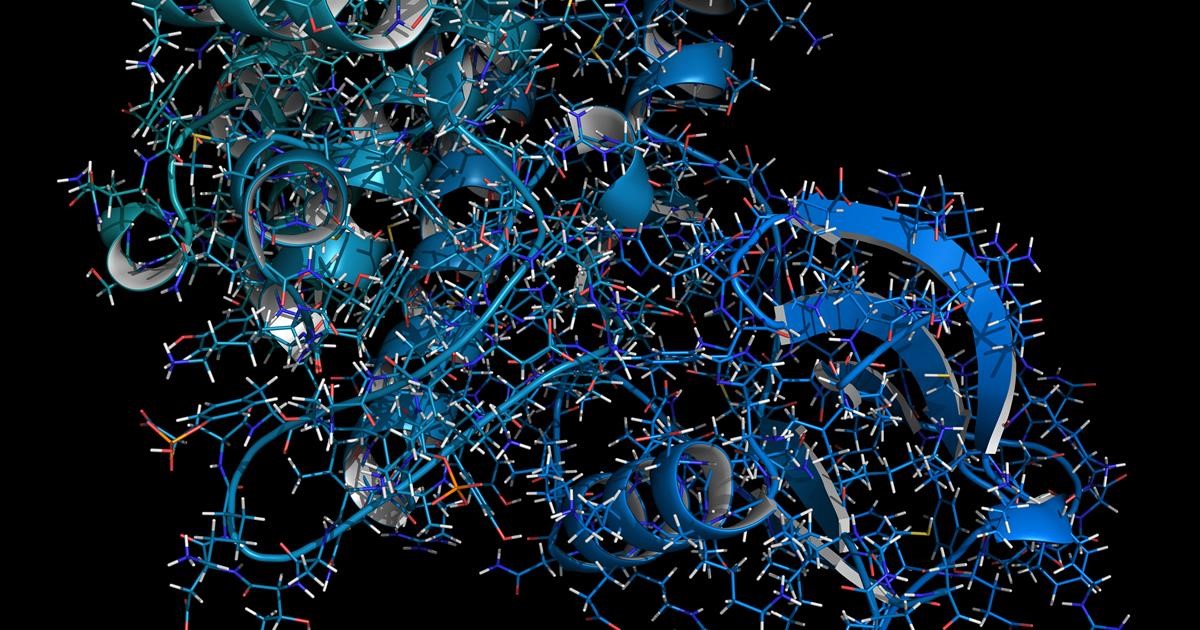
Targeted Therapies
Recent advances in molecular biology and immunology have paved the way for the development of targeted therapies. These therapies aim to specifically modulate the components of the immune system involved in the pathogenesis of autoimmune diseases, thereby reducing disease activity while minimizing side effects.
Janus Kinase (JAK) Inhibitors
One of the most notable advancements in targeted therapies is the development of Janus kinase (JAK) inhibitors. JAK inhibitors, such as tofacitinib and baricitinib, have shown efficacy in treating rheumatoid arthritis and other autoimmune diseases by inhibiting the JAK-STAT signaling pathway, which is crucial for the activation of immune cells. These small molecule inhibitors offer an oral alternative to traditional biologics and have demonstrated significant clinical benefits in reducing disease activity and improving patient outcomes.
Sphingosine-1-Phosphate (S1P) Receptor Modulators
Another promising class of targeted therapies is sphingosine-1-phosphate (S1P) receptor modulators. Fingolimod, an S1P receptor modulator, has been approved for the treatment of multiple sclerosis. By preventing the egress of lymphocytes from lymph nodes, fingolimod reduces the number of autoreactive immune cells in the central nervous system, thereby decreasing inflammation and disease progression.
Biologics
Biologic therapies have revolutionized the treatment of autoimmune diseases by specifically targeting cytokines, cell surface molecules, and other immune system components involved in the disease process. These therapies are typically monoclonal antibodies or fusion proteins that can precisely modulate the immune response.
Tumor Necrosis Factor (TNF) Inhibitors
Tumor necrosis factor (TNF) inhibitors, such as infliximab, adalimumab, and etanercept, were among the first biologics to be approved for the treatment of autoimmune diseases. TNF is a pro-inflammatory cytokine that plays a pivotal role in the pathogenesis of diseases like rheumatoid arthritis and Crohn’s disease. By neutralizing TNF, these biologics can effectively reduce inflammation and disease activity.
Interleukin (IL) Inhibitors
Interleukin inhibitors have also shown great promise in treating autoimmune diseases. For instance, IL-6 inhibitors like tocilizumab have been approved for rheumatoid arthritis, while IL-17 inhibitors such as secukinumab are used in the treatment of psoriasis and ankylosing spondylitis. These therapies work by blocking the activity of specific interleukins that drive inflammation and autoimmune responses.
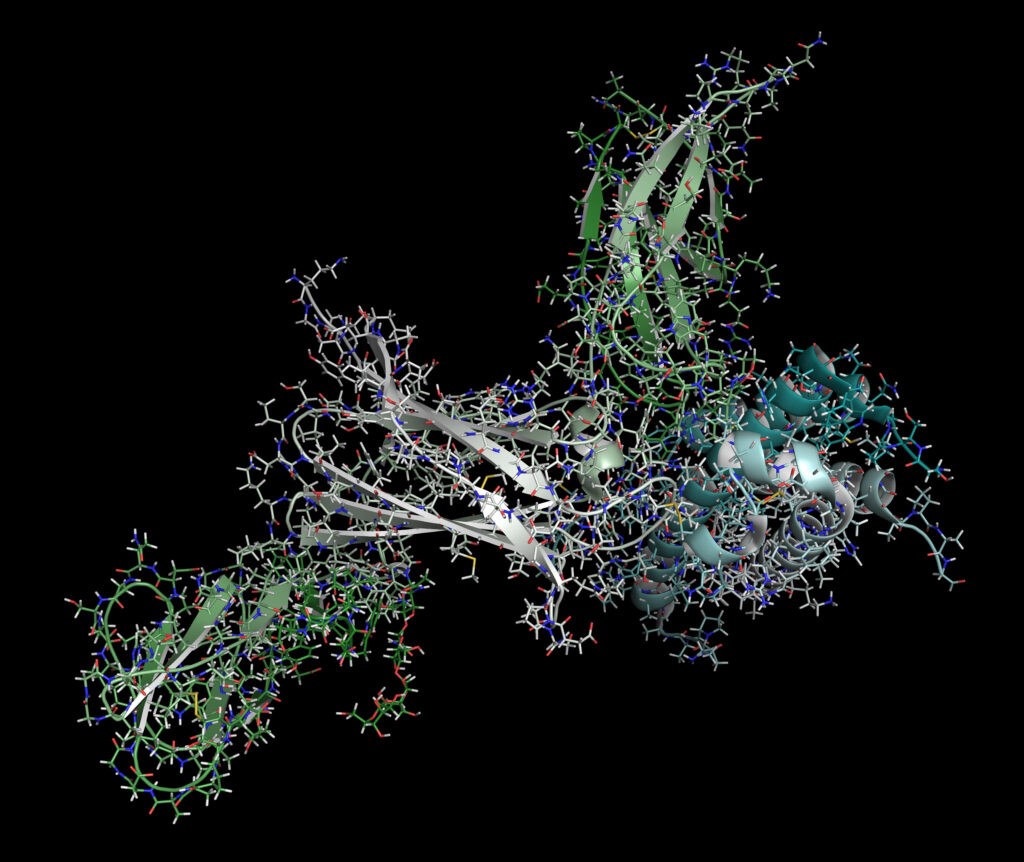
Personalized Medicine
The advent of personalized medicine has the potential to transform the treatment landscape for autoimmune diseases. Personalized medicine involves tailoring treatment strategies to the individual patient’s genetic, molecular, and clinical profile, thereby optimizing therapeutic efficacy and minimizing adverse effects.
Biomarkers
The identification of biomarkers has been a critical step in the development of personalized medicine for autoimmune diseases. Biomarkers can help predict disease progression, treatment response, and potential side effects. For example, the presence of specific autoantibodies can guide the selection of targeted therapies in diseases like rheumatoid arthritis and systemic lupus erythematosus.
Genomic Medicine
Advances in genomic medicine have also contributed to personalized treatment approaches. Genetic studies have identified numerous susceptibility loci associated with autoimmune diseases, providing insights into disease mechanisms and potential therapeutic targets. Whole genome sequencing and other genomic technologies are increasingly being used to identify genetic variants that influence treatment response, enabling more precise and effective interventions.
Conclusion
The treatment landscape for autoimmune diseases has evolved significantly, driven by advances in targeted therapies, biologics, and personalized medicine. These innovations have improved our ability to modulate the immune system with greater specificity, reducing disease activity and enhancing patient outcomes. As our understanding of the molecular and genetic underpinnings of autoimmune diseases continues to grow, further breakthroughs in treatment are anticipated. The ongoing research and development efforts hold the promise of more effective, safer, and personalized therapeutic options for patients suffering from these debilitating conditions.
In summary, the future of autoimmune disease treatment is bright, with targeted therapies, biologics, and personalized medicine leading the way. These advances not only offer hope for better disease management but also underscore the importance of continued investment in research and innovation to address the unmet needs of patients with autoimmune diseases.