Introduction
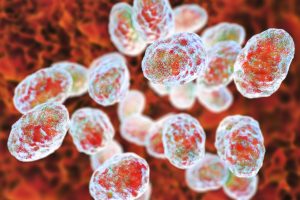
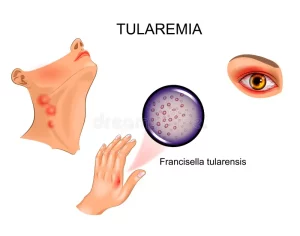
Tularemia, caused by the bacterium Francisella tularensis (F. tularensis), is a highly infectious disease that can have severe consequences if not treated promptly. Commonly known as “rabbit fever” or “deer fly fever,” tularemia spreads from animals to humans through various means, including insect bites, contact with infected animals, and contaminated water or food. Understanding the nuances of this illness, its symptoms, diagnosis, treatment, and preventive measures is crucial for safeguarding public health.
Overview
Tularemia is a zoonotic disease, meaning it can be transmitted between animals and humans. F. tularensis, the causative agent, induces painful swelling of lymph nodes and manifests in different ways depending on the site of infection. Whether it affects the skin, eyes, throat, lungs, or intestines, tularemia requires prompt attention and antibiotic treatment for optimal recovery.
Symptoms and Causes
Understanding the signs and symptoms of tularemia is essential for early detection and intervention. The disease has various forms, each with its own set of symptoms:
- Ulceroglandular Tularemia:
- Fever.
- Swollen and painful lymph nodes.
- Open wound (ulcer) at the site of infection.
- Glandular Tularemia:
- Similar to ulceroglandular tularemia but primarily affects lymph nodes.
- Caused by tick bites or direct contact with infected animals.
- Oculoglandular Tularemia:
- Eye pain.
- Watery eyes.
- Sensitivity to light (photophobia).
- Swollen lymph nodes around the eyes or neck.
- Corneal ulceration.
- Oropharyngeal Tularemia:
- Fever.
- Severe sore throat.
- Swollen, red throat with white patches.
- Digestive symptoms like vomiting, diarrhea, and abdominal pain.
- Pneumonic Tularemia:
- Fever.
- Cough.
- Shortness of breath.
- Chest pain or tightness.
- Muscle aches.
- Skin rash (erythema nodosum).
- Coughing up blood (hemoptysis).
- Typhoidal Tularemia:
- High fever.
- Chills.
- Headache.
- Loss of appetite.
- Muscle aches.
- Sore throat.
- Abdominal pain.
- Diarrhea.
- Nausea or vomiting.
- Confusion.
The incubation period, the time between exposure and symptom onset, is typically three to five days, but some individuals may remain asymptomatic for up to two weeks.
Comparative Table: Tularemia vs. Lyme Disease
| Feature | Tularemia | Lyme Disease |
|---|---|---|
| Causative Agent | F. tularensis | Borrelia burgdorferi |
| Transmission | Infected animals, insects | Tick bites |
| Contagious | Not contagious | Not contagious |
| Severity | Can be life-threatening | Usually not life-threatening |
| Geographic Distribution | Widespread, especially in central U.S. | More widespread globally |
Diagnosis and Tests
Diagnosing tularemia involves a thorough examination, symptom inquiry, and various tests to confirm the presence of F. tularensis. Common diagnostic procedures include:
- Blood Tests:
- A blood sample is taken and sent to a lab to check for signs of tularemia. It may require repeated testing as F. tularensis is slow-growing.
- Biopsy:
- If large lymph nodes or ulcers are present, a tissue sample may be taken for biopsy to test for F. tularensis.
- Nasal or Throat Swab:
- Using a soft-tipped swab, a sample of mucus from the nose or throat is collected and tested for F. tularensis.
- Pleural Fluid Test (Thoracentesis):
- If fluid is present around the lungs, a sample is taken during thoracentesis and tested for F. tularensis.

Management and Treatment
Early and effective treatment is paramount in managing tularemia. Broad-spectrum antibiotics such as streptomycin, gentamicin, doxycycline, azithromycin, ciprofloxacin, or levofloxacin are administered either through injection or oral intake. Antibiotics may be prescribed even before test results are available to prevent the progression of the illness.
Tularemia is curable in humans, and the prescribed antibiotics aim to eradicate the bacteria from the body. However, it’s crucial to complete the entire course of antibiotics as stopping early may allow residual bacteria to cause a relapse.
In addition to antibiotics, managing symptoms at home may be possible. Patients should follow healthcare provider recommendations and inquire about over-the-counter medications or therapies to alleviate specific symptoms.
Prevention
Reducing the risk of tularemia involves adopting preventive measures:
- Protective Clothing:
- Wear clothing that covers exposed skin, especially in outdoor environments with ticks or insects.
- Insect Repellent:
- Use bug spray with DEET to ward off insects.
- Tick Checks:
- Regularly check yourself and pets for ticks, especially in areas that are challenging to see, such as the scalp.
- Pet Supervision:
- Supervise pets when outdoors to prevent bites from infected animals.
- Safe Handling of Animals:
- Wear gloves when handling animals, and avoid picking up wild animals with bare hands.
- Safe Food Practices:
- Cook meat thoroughly and practice proper hand hygiene to prevent foodborne transmission.
- Water Safety:
- Avoid drinking untreated water to prevent waterborne transmission.
- Machinery Caution:
- Exercise caution around animal carcasses to prevent aerosolized particles. Wearing a mask during activities like mowing may offer additional protection.
Individuals with potential exposure to tularemia should consult healthcare providers and treatment for other health problems about the need for preventive antibiotics.
Conclusion
Tularemia, though relatively rare with fewer than 300 cases reported annually in the U.S., demands attention due to its potential severity. Understanding its various forms, symptoms, diagnostic procedures, and preventive measures empowers individuals to protect themselves and their communities. Early recognition and appropriate treatment play a pivotal role in mitigating the impact of tularemia on public health.