Introduction
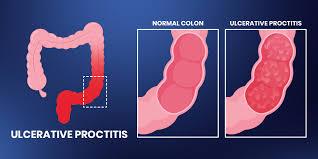
Living with an inflammatory bowel condition can be challenging, and two conditions often discussed together are ulcerative proctitis and ulcerative colitis. While they share similarities, they differ in severity, location, and treatment approaches. Understanding these differences is critical to finding effective relief and planning long-term management. Many patients often wonder about Ulcerative Proctitis vs Colitis Symptoms, treatment strategies, and whether one can progress into the other. In this article, we’ll compare the conditions, explore treatment options, and highlight strategies for living better with each.
Understanding the Basics: What Is Ulcerative Colitis?
Ulcerative colitis is a chronic inflammatory bowel disease (IBD) that causes persistent inflammation and ulcers in the lining of the colon. It typically begins in the rectum and extends upward, affecting varying lengths of the colon. Symptoms often include:
- Abdominal pain and cramping
- Persistent diarrhea (sometimes with blood)
- Urgency to pass stools
- Weight loss and fatigue
People frequently ask, Is ulcerative proctitis the same as ulcerative colitis? The answer is no. Ulcerative proctitis is a subtype of ulcerative colitis, characterized by inflammation limited to the rectum.
What Is Ulcerative Proctitis?
Ulcerative proctitis is the mildest form of ulcerative colitis, restricted to the rectal area. Its symptoms can be milder but still disruptive. Common signs include:
- Rectal bleeding
- Urgency to pass stool
- Mucus discharge
- Pain or discomfort during bowel movements
Because it is localized, treatment strategies may differ, and some patients report searching for answers on how I cured my proctitis through lifestyle, diet, or medical therapy.
Key Differences Between Ulcerative Proctitis and Colitis
| Feature | Ulcerative Proctitis | Ulcerative Colitis |
|---|---|---|
| Affected Area | Rectum only | Rectum + part or all of colon |
| Severity | Milder | Can be severe |
| Common Symptoms | Rectal bleeding, urgency | Diarrhea, cramps, fatigue |
| Risk of Complications | Low | Higher |
| Progression | May stay limited or spread | Often spreads if untreated |
Understanding these differences helps in choosing the right treatment and managing the condition effectively.
Causes and Risk Factors
Both conditions are caused by problems with the immune system. Instead of protecting the body, the immune system attacks the lining of the colon or rectum, causing inflammation.
Common Causes and Triggers:
- Genetics (family history of IBD)
- Immune system disorders
- Poor diet or changes in gut bacteria
- Stress and anxiety (may worsen symptoms)
- Smoking (linked more with Crohn’s but still affects IBD)
It’s important to understand that while stress and food can make symptoms worse, they are not direct causes of these diseases.
Proctitis vs Colitis Symptoms
While both conditions involve inflammation in the digestive tract, the extent of inflammation differs.
- Ulcerative Proctitis Symptoms: Localized to the rectum. Rectal bleeding, mucus, and urgency are more common.
- Ulcerative Colitis Symptoms: Broader, affecting the colon. Includes diarrhea, abdominal cramping, systemic fatigue, and weight loss.
This difference in symptoms is important because it influences treatment strategies and monitoring.
Can Ulcerative Proctitis Turn into Ulcerative Colitis?
A question often asked by patients is: Can ulcerative proctitis turn into ulcerative colitis?
In some cases, yes. Research suggests that up to 30% of people with ulcerative proctitis may eventually experience inflammation that spreads further into the colon. This progression underscores the importance of early treatment and regular medical follow-up.
Also Read: Why fitness and self-care go hand in hand?
Treatment Options for Ulcerative Proctitis and Ulcerative Colitis
1. Medications
Treatment usually begins with medication.
- Topical Therapies: Suppositories and enemas containing mesalamine or corticosteroids help directly target rectal inflammation.
- Oral Medications: Amino salicylates, immunosuppressants, and biologics are often used when inflammation extends beyond the rectum and into the colon.
- Advanced Therapies: For patients with resistant disease, biologics and JAK inhibitors are considered among the latest treatments for ulcerative colitis.
2. Dietary Adjustments
While no food directly causes ulcerative colitis, diet plays a big role in symptom management. Following an ulcerative colitis diet tailored to reduce triggers can help minimize flare-ups. Patients often experiment with:
- Low-residue or low-fiber diets during flares
- Avoiding caffeine, alcohol, and high-fat foods
- Staying hydrated
- Including probiotic-rich foods to support gut health
3. Lifestyle Strategies
- Stress management: Stress can exacerbate symptoms, so incorporating mindfulness, yoga, or meditation can be beneficial.
- Regular check-ups: Monitoring disease progression ensures timely adjustments to treatment.
- Exercise: Engaging in gentle physical activity may help reduce fatigue and support mental health.
4. Surgery (For Severe Cases)
In advanced ulcerative colitis cases where medication fails, surgery may be an option. While many people search for a permanent cure for ulcerative colitis, surgery (removing the colon) is currently the only known cure. However, it’s not always necessary, and many manage symptoms effectively with medical therapy.
Proctitis Ulcerative Colitis Treatment: Tailored Approaches
Since ulcerative proctitis is more localized, treatment strategies are often more targeted compared to full colitis. Common approaches include:
- Mesalamine suppositories for direct anti-inflammatory relief
- Steroid enemas for short-term flare control
- Escalation to oral or systemic medications if the disease progresses
Meanwhile, ulcerative colitis patients often require broader treatments, such as systemic biologics or immunomodulators. This makes proctitis treatment for ulcerative colitis a more localized and potentially less intensive process, although regular monitoring is still essential.
Patient Experiences: “How I Cured My Proctitis”
Many patients share personal stories online about finding what works for them. While there isn’t a one-size-fits-all cure, some strategies reported by patients include:
- Combining medication with dietary changes
- Using rectal therapies consistently
- Managing stress effectively
- Exploring complementary therapies like probiotics
It’s important to note that while some individuals say, “How I cured my proctitis,” medical guidance should always be part of treatment planning, since these conditions can change or progress.
The Role of Clinical Research
New treatments continue to emerge. From biologics to novel small-molecule drugs, researchers are constantly investigating what is the latest treatment for ulcerative colitis? Clinical research is vital for offering hope to patients seeking a better quality of life with fewer side effects.
Treatment Goals
The main goals of treatment for both ulcerative proctitis and ulcerative colitis are to:
- Reduce inflammation
- Control symptoms
- Prevent flare-ups
- Improve quality of life
- Avoid complications
Although they share the same goals, the treatment approach may vary depending on how much of the colon is involved.
Conclusion
Both ulcerative proctitis and ulcerative colitis are chronic inflammatory conditions, but they differ in severity, location, and treatment requirements. By understanding the symptoms of proctitis vs. colitis, patients can work with healthcare providers to tailor their treatment. For some, proctitis may remain mild and localized, while for others, the inflammation may spread to involve the entire colon, resulting in full-blown colitis.
Managing these conditions often requires a combination of medication, diet adjustments, lifestyle strategies, and ongoing monitoring. While there is currently no universal permanent cure for ulcerative colitis, effective treatment strategies can significantly improve quality of life. If you or a loved one is navigating these conditions, staying informed and exploring advanced therapies through Ulcerative Proctitis Clinical Trials can open doors to innovative treatment options and better outcomes.