Jaundice
Jaundice, a condition marked by the yellowish pigmentation of the sclera and skin, is a result of elevated levels of bilirubin in the body. This article delves into the multifaceted aspects of jaundice, elucidating its causes, symptoms, and the diagnostic processes involved.

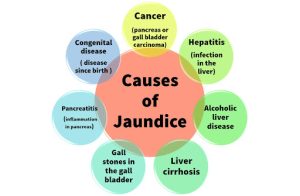
Understanding the Causes of Jaundice
Jaundice manifests due to imbalances in four primary areas:
1. Conditions Affecting Red Blood Cells
An increased breakdown of red blood cells leads to heightened bilirubin levels. Genetic diseases like sickle cell anemia and thalassemia, along with conditions such as hemolytic uremic syndrome and malaria, contribute to this mechanism.
2. Conditions Affecting Liver Cells
Various conditions impact the functionality of liver cells, causing them to struggle with bilirubin processing. Hepatitis, cirrhosis, and inherited enzyme defects, including Gilbert’s syndrome and Dubin-Johnson syndrome, can result in jaundice.
3. Conditions Affecting Tiny Bile Ducts
Damage or narrowing of the tiny bile ducts within the liver restricts the flow of bile, leading to bilirubin accumulation. Primary biliary cirrhosis and primary sclerosing cholangitis are among the conditions affecting these ducts.
4. Conditions Affecting the Common Bile Duct
Obstruction of the common bile duct results in bile, containing bilirubin, seeping into the bloodstream. Causes include gallstones, pancreatic cancer, and inflammation of the pancreas.
The Intricacies of Jaundice – Decoding Bilirubin Processing
Bilirubin, a byproduct of red blood cell breakdown, undergoes processing in the liver. The liver converts it into conjugated bilirubin, which is water-soluble and then passed into the bile ducts. Bile, containing bilirubin, travels through the liver’s ducts into the common bile duct and eventually reaches the small intestine.
Unraveling Jaundice Symptoms
The onset of jaundice is often evident in the whites of the eyes turning yellow. With higher bilirubin levels, the skin also undergoes discoloration. Additional symptoms vary based on the cause and may include fatigue, abdominal pain, weight loss, vomiting, itching, fever, pale stools, and dark urine.
Navigating the Diagnostic Landscape for Jaundice
When jaundice symptoms arise, seeking medical attention is crucial for a comprehensive evaluation. Diagnostic processes encompass various tests:
- Blood Tests: These distinguish between unconjugated and conjugated bilirubin, aiding in narrowing down potential causes. Liver function tests measure enzymes, indicating liver inflammation or functionality.
- Urine Tests: Identifying raised levels of certain chemicals helps narrow down potential causes.
- Imaging Techniques: Ultrasound scans and magnetic resonance imaging (MRI) can pinpoint blockages or abnormalities in the liver, common bile duct, and pancreas. A liver biopsy may be performed for microscopic examination.
- Extended Tests: In cases where the diagnosis remains uncertain, more complex tests may be necessary for a conclusive understanding.

Jaundice in Newborns: An In-Depth Look
Jaundice in newborns can be categorized into physiological jaundice, typically resolving within the first week, and other causes. Medical attention is advised for persistent or early-onset jaundice, as it may indicate underlying issues.
Treatment Approaches for Jaundice
Treatment for jaundice hinges on addressing the root cause. There is no specific treatment for jaundice itself, emphasizing the importance of identifying and managing the underlying condition. Specific diseases contributing to jaundice, such as hepatitis, gallstones, and liver cancer, require targeted treatment.
Understanding the intricacies of jaundice, from its origins to symptoms and diagnosis, empowers individuals to seek timely medical intervention. If jaundice symptoms arise, consulting a healthcare professional for a comprehensive assessment is paramount for accurate diagnosis and appropriate management.










