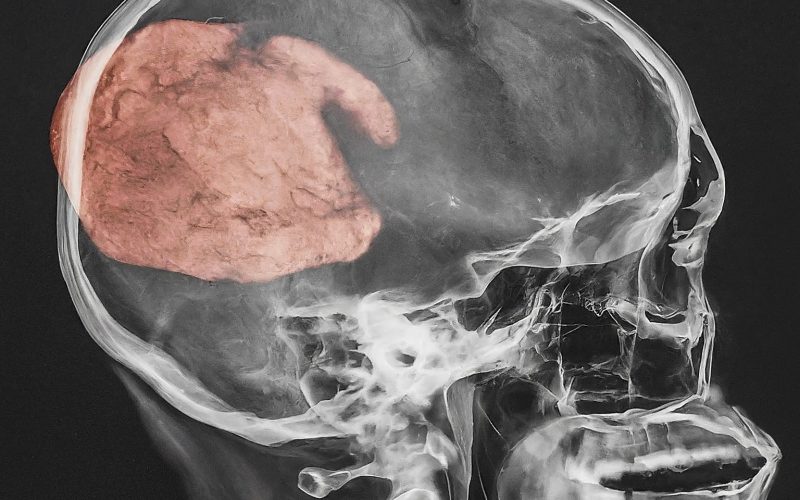
New Technique Could Help Treat Aggressive Brain Tumors
In the ongoing battle against aggressive brain tumors, medical researchers and oncologists are constantly in pursuit of more effective treatment methods. A groundbreaking technique has emerged, showing promise in the treatment of these formidable cancers. This innovative approach leverages advanced technologies and novel therapeutic strategies to target tumors more precisely and with potentially fewer side effects.
Understanding the Challenge of Brain Tumors
Brain tumors, particularly malignant types like glioblastoma, are notoriously difficult to treat. Their location within the critical and complex environment of the brain makes surgical interventions risky, while their tendency to infiltrate brain tissue complicates complete removal and enhances the likelihood of recurrence. Traditional treatments such as chemotherapy, radiation therapy, and surgery have reached a plateau in effectiveness, with significant side effects and often limited improvement in survival rates.
The Emergence of a New Technique
The new technique, which is still in the experimental stages, involves a combination of targeted drug delivery systems and genetic engineering. The primary focus is on improving the precision of treatment delivery, thereby maximizing the therapeutic impact on the tumor while minimizing damage to surrounding healthy brain tissues.
Targeted Drug Delivery Systems
One of the pillars of this new technique is the use of nanoparticles for targeted drug delivery. These microscopic particles are designed to bypass normal biological barriers and deliver chemotherapeutic agents directly to the tumor cells. This method not only enhances the drug’s efficacy but also reduces the systemic side effects typically associated with chemotherapy.
By conjugating these nanoparticles with specific ligands or antibodies that recognize and bind to tumor-specific markers, the treatment becomes highly selective for cancer cells. This specificity is crucial in preserving the integrity and function of the brain’s normal cells, which are often inadvertently affected by conventional treatments.
Genetic Engineering and Personalized Medicine
The second critical component of this technique is genetic engineering, which plays a significant role in customizing treatments for individual patients. By analyzing the genetic makeup of a patient’s tumor, oncologists can identify unique mutations and tailor therapies that specifically target those abnormalities.
Recent advances in CRISPR-Cas9 technology have enabled precise edits to DNA, providing opportunities to disable or correct genes that drive tumor growth. In the context of brain tumors, this could mean disrupting the genetic pathways that allow cancer cells to proliferate uncontrollably or resist standard therapies.
Clinical Trials and Preliminary Results
Early-stage clinical trials of this new technique have shown promising results. In one study, patients with recurrent glioblastoma treated with nanoparticle-mediated targeted therapy showed a statistically significant improvement in median survival rates compared to those receiving conventional treatment. Moreover, the targeted approach has led to fewer instances of debilitating side effects, such as neurotoxicity, that are common with traditional therapies.

Future Directions and Challenges
While the initial findings are encouraging, there are several hurdles to overcome before this technique can become a standard treatment option. One of the major challenges is the heterogeneity of brain tumors. Each tumor can vary significantly in its genetic profile, not only between different patients but also within the same tumor. This variability requires highly personalized approaches, which can be complex and costly to implement on a larger scale.
Another issue is the potential for resistance to therapy. As with many forms of cancer, there is a risk that brain tumor cells will adapt and develop resistance to targeted therapies. Ongoing research is focused on understanding these mechanisms of resistance and finding ways to counteract them.
Conclusion
The development of this new technique represents a significant leap forward in the treatment of aggressive brain tumors. By integrating targeted drug delivery systems with the precision of genetic engineering, researchers are paving the way for more effective and less harmful therapies. However, the path from experimental to routine clinical practice is fraught with challenges that must be carefully navigated through continued research, collaboration, and innovation.
As we move forward, it is crucial that the scientific community remains committed to refining these techniques, ensuring their accessibility, and ultimately, improving the prognosis for patients afflicted with these devastating diseases. The journey is long, but the potential benefits for patient care and survival are profound, marking a hopeful new chapter in the fight against brain tumors.